
|
African Health Sciences
Makerere University Medical School
ISSN: 1680-6905 EISSN: 1729-0503
Vol. 2, Num. 3, 2002, pp. 124-126
|
African Health Sciences, Vol. 2, No. 3, December, 2002, pp. 124-126
A 14-year-old Nigerian female with idiopathic intracranial hypertension (Pseudotumor cerebri or benign intracranial hypertension)
A.C Onwuchekwa*, C.N. Nwankwo**, E.N. Chapp-Jumbo*
* Neurology Unit, Department of Medicine, University of Port Harcourt & University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria.
** Department of Radiology, University of Port Harcourt & University of Harcourt Teaching Hospital, Port Harcourt, Nigeria.
Authors for Correspondences Dr E.N.Chapp-Jumbo Department of Medicine, University
of Port Harcourt & University of Port Harcourt
Teaching Hospital, Port Harcourt, Nigeria.
Email: chap.jumbo@mwkl.co.uk
Code Number: hs02053
ABSTRACT
A 14-year-old secondary school girl presented with acute onset severe generalized headache associated with vomiting and diplopia. These followed an initial fever, which responded to chloroquine. She had been on perflacine for a left knee septic arthritis until onset of her symptoms. The main findings on physical examination were mild obesity, left abducent nerve palsy, bilateral papilledema and evidence of resolving arthritis of her left knee. The results of her investigations, including a brain CT scan were within normal limits. A diagnosis of IIH was made. She responded satisfactorily to oral acetazolamide with complete resolution of her symptoms and signs within 12 days of hospitalization and 2 weeks of follow-up.
BACKGROUND & OBJECTIVE
Idiopathic intra-cranial hypertension (IIH) is not
commonly encountered and when it is, delay in
initiation of medical treatment can lead to
permanent visual impairment. It is a diagnosis of
exclusion. This is the first reported case in Port
Harcourt, Nigeria and it serves to create awareness
and the importance of early treatment.
CASE REPORT
J.A. was a 14-year-old Nigerian female secondary
school student referred from a peripheral primary
health-care center on the 23/03/2001 with the
complaints of severe generalized, throbbing
headaches for 6 days, vomiting for 3 days and
diplopia for one day, prior to presentation. The
headaches were worse with straining and in the
mornings with no associated neck pains. There was
an initial fever that subsided with antimalarial
treatment. She started vomiting three days into her
illness and this was non-projectile, worse in the
mornings and not proceeded by nausea. Diplopia
was observed a day before presentation and worse
with attempting to look towards her left. She had
been taking oral pefloxacin mesylate (peflacine) for septic arthritis of her left knee secondary to trauma
diagnosed a month earlier, until the onset of her illness.
She denied travels to the meningitis belt of the country in
the recent past, use of oral contraceptives or sexual
exposure. She does not take alcohol or use tobacco in any
form. There is no past history of similar illness or family
history of migrainous headaches, diabetes, sickle cell
disease or brain tumors.
Physical examination showed that she was obese
with a BMI of 30.6, conscious and alert, photophobic,
afebrile, not pale, not jaundiced, acyanotic, mildly
dehydrated and breathing normally. Her pulse rate was
72/minute and BP 120/70mmHg. She had no neck
stiffness; Kernig’s and Brundzinsky’s signs were negative.
Pupillary reaction to light and accommodation was normal
bilaterally and there were no visual field defects. She had
left abducent nerve palsy and fundocospy revealed both
fundi to have pink discs with blurred margins and engorged
vessels. The visual disc: cup ratio was 0.3 bilaterally and
there was good macular reflex and background bilaterally.
These findings were in keeping with bilateral papilloedema.
Her muscle tone, power and reflexes were normal in all
limbs and so were her sensation and coordination. Further
systemic examination was unremarkable except for a mildly
swollen and tender left knee joint with no redness or
warmth but with some limitation of movement.
A diagnosis of a Raised Intracranial Pressure
?cause, to rule out Idiopathic Intracranial Hypertension
(IIH) or Metastatic Brain Abscess was made and she was
admitted for investigation and treatment.
Chest X-ray was within normal limits.
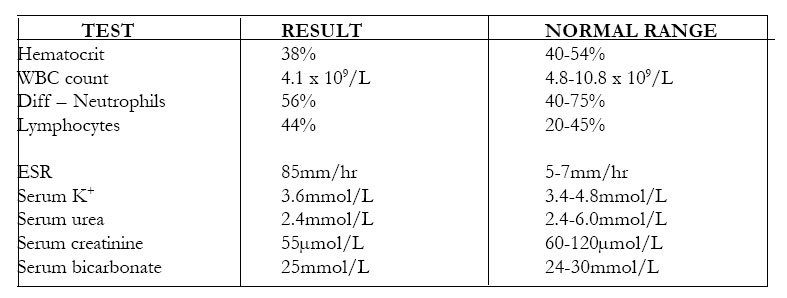
The results of her investigations were as shown:
Brain CT scan revealed a normal cranial vault, sella and suture lines. The brain slices showed normal tissues and ventricular systems and there were no intracranial mass lesions.
X-rays of the left knee joint revealed a narrowing of the medial tibio-femoral and patello-femoral joint spaces with spiking of the tibial spine, suggestive of secondary osteoarthritis.
Urinalysis showed normal findings.
Lumbar puncture was not done because of the signs of raised intracranial pressure and the diagnosis was uncertain initially.
A definitive diagnosis of Idiopathic intracranial hypertension was eventually made and the patient was placed on a weight-reducing diet, oral actazolamide 50mg tds and analgesics. She responded satisfactorily on the above regimen with the resolution of her headaches and vomiting, while the ocular palsy gradually resolved and she was discharged on the 4/4/2001 after 12days of hospitalization. On follow-up visit two weeks later, she had completely recovered without any sequelae and her fundal re-examination and visual fields were normal.
DISCUSSION
This is the first reported case of IIH in UPTH, PH. It is not commonly encountered. A review of neurological admissions from Kenya1 showed no reported case of IIA. This rare neurological disease entity was first recognized by Quinke in 1897 2. It has previously been described by various terminologies such as toxic hydrocephalus, otitic hydrocephalus, hypertensive meningeal hydrops, pseudoabscess, pseudotumor cerebri and lately benign intracranial hypertension in 1955. However the name IIH has been suggested because about 20-50% of cases experience permanent visual impairment 2.
No age group is immune to the disease but there is a female preponderance in a ratio of M: F, 1:3. There is a strong association with obesity and weight gain during the twelve months prior to diagnosis. Patients present with symptoms similar to those of our patient, including infrequent ones such as intermittent and paroxysmal alteration of consciousness, tinnitus and paraesthesias; seizures are thought never to be part of the classic symptoms. The most consistent finding is papilledema and there may also be ocular palsies, both present in our patient. The diagnostic criteria 2,3,4 include symptoms related to intracranial hypertension – headache, in the absence of focal neurological symptoms; signs related to intracranial hypertension – papilledema and enlarged blind spots in the absence of focal neurological signs except for 6th nerve palsy; documented intracranial hypertension; normal CSF cellular content and biochemistry and a normal cranial CT or MRI. Our patient met these diagnostic criteria, except the CSF findings.
The diagnosis of IIH is one of exclusion. The diagnostic studies required include plain skull radiographs, which shows sutural diastasis in the young, in addition to demineralization of the sella. It is diagnostic of intracranial hypertension, but this is seen only in 10% of patients 3. Electroencephalogram (EEG) is normal in nearly 90% of adult patients but there is a higher incidence of abnormal studies in patients below 20 years of age 3. Isotope brain scans are normal in a vast majority of patients. CT scan and MRI are usually normal while CSF findings include an elevated pressure, usually greater then 250 mm H20 with variable levels of protein 5.
There are numbers of clinical conditions which meet the modified Dandy’s criteria for association with IIH2, these include hematological disorders such as iron deficiency anemia, pernicious anemia and polycythemia rubra vera; endocrine disorders like corticosteroid deficiencies, corticosteroid excess, thyroid and parathyroid diseases and pituitary diseases such adenomas and acromegaly; metabolic or nutritional disorders such as cystic fibrosis, galactokinase, galactosemia, hyper- or hypovitaminosis A, vitamin D deficiencies and rickets; drugs such as anabolic steroids, phenytoin, chlorpromazine, lithium carbonate, tetracycline, nalidixic acid, nitrofurantoin, sulfamethoxazole, amiodarone, and indomethacin. Our patient was taking a quinolone, pefloxacin, of which nalidixic acid is a member, until the onset of her illness. It is difficult to say the role of this drug in the genesis of her illness as the other strong factors like her gender and obesity were at play. Some disease conditions, which are also associated with this entity according to the modified Dandy’s criteria, include sarcoidosis, systemic lupus erythematosis (SLE), any obstruction to cranial venous outflow such as head injury, chronic ear infections and obstruction of flow through the arachnoid granulations.
The treatment of IIH requires critical decisions relating to timing, which should be before the onset of permanent optic nerve death and the type of therapy. Medical treatment should be instituted first with weight reducing diet, acetazolamide 2-4g/day. Other drugs that have been used with success include glycerol 0.25-1.0g/ kg/dose bd or tds, frusemide 20-60 mg daily and paradoxically, corticosteroids 40-60 mg/day. Other interventions found useful in selected cases include, serial lumbar punctures twice weekly initially then weekly until resolution of signs and symptoms of disease 2. Surgery is indicated when existing visual field defects enlarge or deepen during the course of medical treatment; when new visual scotomas occur; when a Marcus-Gunn’s pupil develops or when visual acuity falls. This usually takes the form of optic nerve sheath incision and CSF shunting 6.
The long-term prognosis in this condition is good as observed in our patient with the exception of permanent visual loss, which has been documented in a sizeable number of patients 2. Poor prognostic factors include an older patient and a female sex and recurrence rate is up to 12% 2.
CONCLUSION
IIH was previously thought to be benign but it is now known to cause permanent visual impairment in 20 –50% of its victims especially when treatment is delayed. This case reminds us of the need to bear in mind, occurrences of ‘rare’ diseases and the importance of prompt initiation of treatment.
REFERENCES:
- Haddock, D R W. Neurological diseases in Tanzania. J Trop Med Hyg 1965: Jul; 161.
- Steven L. Wald. Disorders of cerebrospinal fluid circulation and brain edema. In Neurology in Clinical Practice. Vol. 2; 2nd edition 1990: 1431-1458.
- Radhakrishnan K, Ahlskog J E, Cross S A et al. Idiopathic Intracranial Hypertension (Pseudotumor cerebri). Arch Neurol 1993; 50: 78 – 80.
- Wall M. Idiopathic Intracranial Hypertension. Neurol Clin 1991; 9: 73 – 95.
- Johnson P K, Corbette J J, Maxner C E. Cerebrospinal fluid protein and opening pressure in Idiopathic Intracranial Hypertension (Pseudotumor cerebri). Neurology 1991; 41: 1040 –1042.
- Spoor T C, Ramocki J M, Madion M P et al. Treatment of pseudotumor cerebri by primary and secondary optic nerve sheath decompression. Am J Ophthalmol 1991; 112: 177 – 185.
Copyright © 2002 - Makerere Medical School, Uganda
|
